“Discovering a skin cancer early can make the difference…
between life and death.”
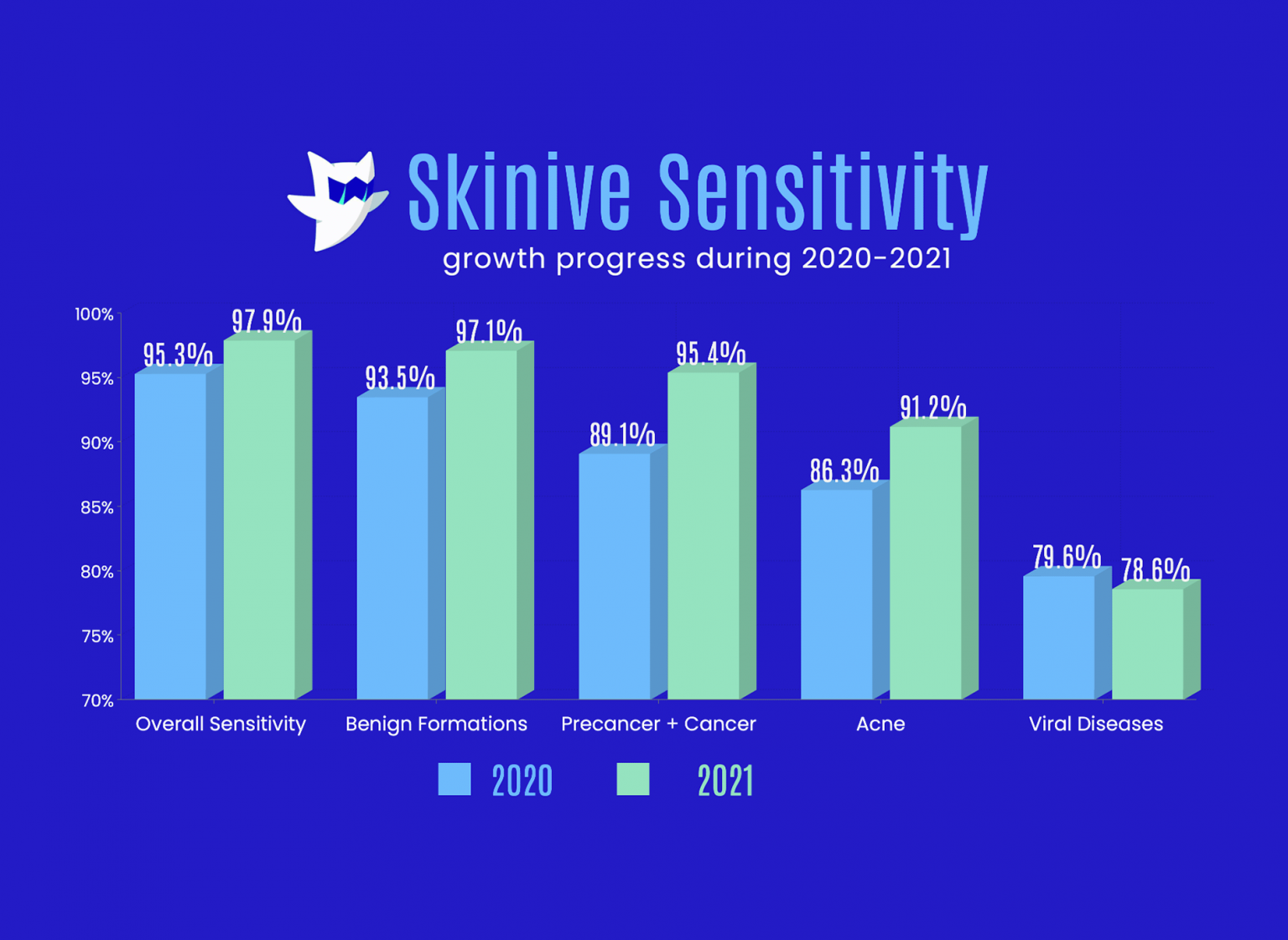
The difference between life and death…” Wow. As frightening as that might be, never underestimate the power that comes with knowing the techniques for early detection. Remember, skin cancer is almost always curable — if it’s detected and removed early. The easiest way to check the health of your moles for cancer risks is to download the Skinive app and do an AI analysis of your skin based on a smartphone photo.
Exams, both personal and professional, are life-and-death important
Besides skin checks at home, schedule regular and as-needed medical skin exams for yourself and your family — especially if any of you is at increased risk for skin cancer.
Annual skin exams by a health care professional have been shown to reduce deaths from melanoma by half.3 If your skin exam wasn’t performed by an actual dermatologist, follow up with one for an evaluation of any suspicious findings. Expect your dermatologist, an MD with specialized education and experience diagnosing and treating skin cancers, to listen carefully to your concerns, perform a thorough skin examination, and clearly communicate findings and recommendations for follow-up.
Monthly personal and annual professional skin checks improve your own, your spouse’s, and your children’s chances for early detection, treatment, and survival of a skin cancer diagnosis.
Do I really need to check my children for skin cancer?
Yes, absolutely
The following facts provided by Dana-Farber on childhood skin cancer are clear: Although rare, children do develop skin cancer — and it’s almost always melanoma — the deadliest of the three most common skin cancers.4
The risk of melanoma increases for those children with the same risk factors as adults (fair skin, sunburns, moles, family history). Moreover, the biggest increase in melanoma diagnoses is in girls 15–19 years old, most likely related to their sunbathing and tanning bed habits as well a seeming reluctance to wear protective clothing.
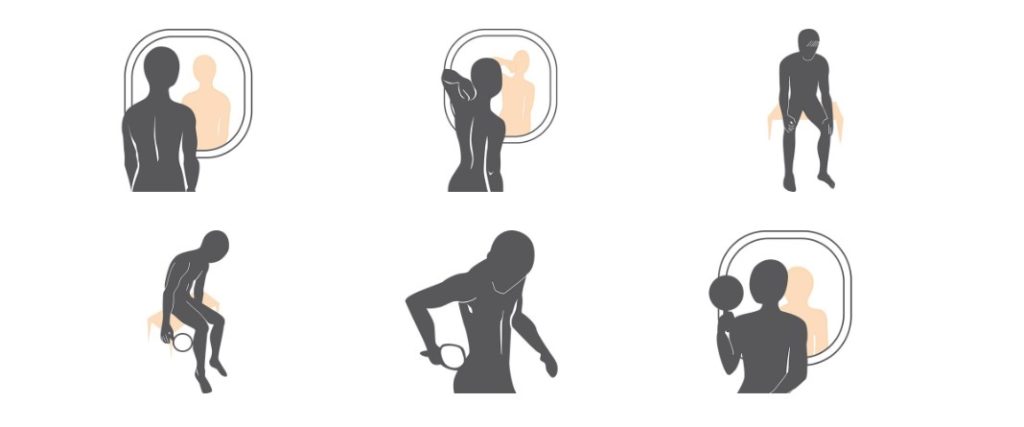
Follow the step by step instructions in this gallery to examine your skin. Take Smartphone shots to use Skinive
If your child falls into an increased risk category, perform their monthly skin checks and schedule them for annual and as-needed skin examinations by a pediatric dermatologist.
Don’t be frightened — you can do this. Read on for the additional information you’ll need to practice good stewardship of your own and your family’s skin health:
- what a suspicious mole or lesion looks like; and
- how to perform a skin check.
When is a mole or lesion suspicious?
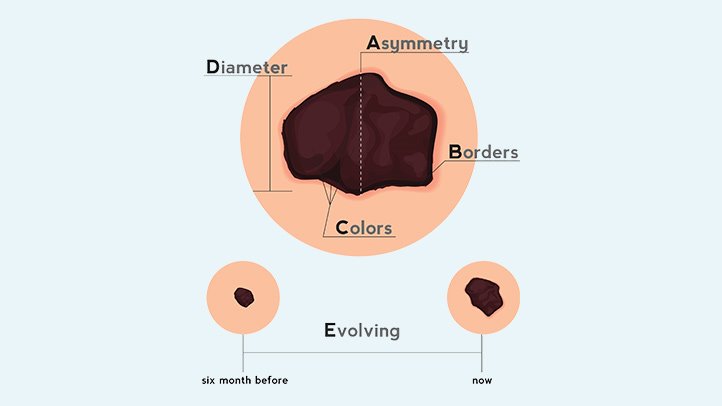
One or more of the following characteristics is highly suggestive of a melanoma, the most lethal skin cancer, and should be immediately evaluated by a dermatologist or, if a child, a pediatric dermatologist. To help you remember these, think ABCDE.
- A=Asymmetry
One half is a different shape from the other. - B=Border
The edges are irregular. - C=Color
There are variations in color (tan, brown, black, red, white) within the borders. Children’s melanoma is more likely to be whitish, yellowish, or red and somewhat wart-like in appearance 5 - D=Diameter
This characteristic is less definitive — while often larger than a pencil eraser, they can be smaller. - E=Evolving
The size, shape, color is changing or there is itching, bleeding or difference from your other moles or lesions.
Of all these characteristics, an evolving or changing mole or lesion is the most suggestive of melanoma. And you are the best person to spot these changes early. Check your skin regularly!
The characteristics of basal cell and squamous cell lesions (the most common and second most common skin cancers) may be only a growth, bump, or sore that is unusual in appearance or does not heal within a month.
The slideshow Precancerous Skin Lesions and skin cancer can help you recognize what you might find during your skin checks.6 For anything that makes you suspicious of skin cancer or pre-cancer, make an appointment with your dermatologist for an immediate evaluation.
How to perform a skin check
What you’ll need
- good lighting;
- a comb or hair dryer to part hair;
- a mirror if you’re checking your own scalp and back surfaces;
- a small flexible plastic or paper millimeter (mm) ruler;
- a flashlight; and
- a means to document what you find (paper, computer, or smartphone app).
Photographing and dating lesions and regions (your back, your chest, your thigh, etc.) is very helpful in documenting your skin status.
Measure lesions and moles using a millimeter (mm) ruler
- from side-to-side first;
- then from top-to-bottom; and finally
- the distance, if any, each is raised on the skin.
What to check
Whether performing skin checks on yourself or family members, leave no areas unexamined. This includes: the scalp and face; the fronts, tops, and backs of ears; around the neck; tops of shoulders; full front and back; as well as both sides from armpits to ankles.
Also check: the sex organs; fronts and backs of arms and legs; tops of hands and feet; and between all fingers and toes.7 8 The palms and soles as well as under and around all nails should be checked by everyone — but are especially important to dark complexioned persons as they are more likely to develop a virulent strain of melanoma in these areas.9 Did I forget anything? Check that too.
The baseline and follow-ups
The first full-body skin check can take quite a while as you are creating a baseline. Try dividing it up: all fronts, hands, and feet one day; then the scalp, all sides, and backs on another (perhaps when you have help).
Follow-up checks — when you’re looking for changes to the already documented moles and lesions or the emergence of new ones — should take only 10–15 minutes.
Keep track of what you find
As you’re checking, record each finding for each family member. You can use preprinted forms or create your own. And, not surprisingly, there’s an app for that.
As your children mature, have them join you, first checking and later recording easy skin findings. This will teach them the habit, the skills, and the importance of regular skin checks.
The skcin.org website provides a useful form to use as you inspect and document lesions and moles.10
Minimize the impact of skin cancer on yourself and your family
The importance of protecting yourself and your family from skin cancer — as well as assuring its early detection and successful treatment — cannot be overstated.
As part of your protection plan, you should:
- mandate, demonstrate, and facilitate avoidance of ultraviolet ray exposure;
- perform thorough monthly skin checks;
- schedule annual medical skin examinations; and
- schedule immediate dermatologic evaluation of any suspicious moles or lesions.
Early discovery of skin cancer can be the difference between office-based surgery and far more invasive treatment, even between life and death. Choose life.
Let’s begin with this: Reducing the risk of — or even preventing — skin cancer for yourself and your children is an achievable goal.1 But not if you remain unaware of the risk factors, or if you treat those risk factors nonchalantly.
The principle risk factor for skin cancer is exposure to ultraviolet (UV) radiation. It also increases your chances for developing serious eye maladies including cataracts and macular degeneration.2 The major source of UV radiation is the sun, followed by other sources such as tanning beds and welding.
So, why aren’t you protecting yourself and your children from UV radiation?
Perhaps you were unfamiliar with the facts about skin and eye damage from UV. Or possibly you knew the facts but thought it was more important to get a tan — thinking you’d look more beautiful, or more virile. Maybe you think it’s uncool to slather up with sunscreen before going outdoors. Or you might have deceived yourself into thinking you’re not at risk for skin cancer, or that it’s too far in the future to worry about.
Or, is it simply that you know the risks and intend to protect yourself but have yet to develop the necessary sun protection habits?
Whatever is preventing you from adopting sun protection as a daily habit needs to change — it is time to protect yourself and your children.
Let’s look at what might be holding you back
Thinking you look better tanned
If you like your appearance with a tan, then opt for a sunless-tanning lotion.3 Used correctly, sunless tanning products can provide the look of a healthful tan — without the UV damage that contributes to early skin wrinkling and sagging, sun spots, and cancer. But remember, a sunless tan does not protect you from UV exposure — or the long term consequences of UV exposure which are not attractive.
Thinking you’re protected by skin color
For dark complexioned persons, you do have additional protection against the most common skin cancers — but, you are not immune. While your risks are lower, unprotected UV radiation still increases your odds for premature skin aging and skin cancer, as well as cataracts and macular degeneration.4
Thinking you can wait until you’re older
Unfortunately, the group with the least protection and the greatest long-term risk is the young. UV radiation exposure is more toxic to the them, and it is cumulative throughout their lifetime. No one should wait to start sun protection until they’re older. Childhood and adolescent UV exposure from sun or tanning beds, when it results in even one or two blistering sunburns, is associated with an increased incidence of all skin cancers, especially the most deadly, melanoma.5 Protect your children.
Thinking it’s too difficult or too complicated
To lower your risk of skin cancer — and your children’s risk — you just need to establish the habit of using UV protection before UV exposure. It’s that simple.
More facts about skin cancer
Let’s review some facts about skin cancer as presented by cancer.org.6 Then, in Part 2, I’ll take a look at sun protection strategies as well as tips for adding those strategies to your daily wellness habits.
There are three common skin cancers
- basal cell,
- squamous cell, and
- melanoma.
The two most prevalent, basal cell and squamous cell, usually found on sun exposed areas of the skin, account for 5.4 million diagnoses in the U.S. each year, with basal cell outnumbering squamous cell, 8 to 2. Even though basal and squamous cell skin cancers are treatable, especially when detected early, they contribute to an estimated 2,000 deaths in the U.S. annually.
Melanoma, the least common of these (1% of all skin cancers), is the most common cause of skin cancer deaths (80%). In 2016, we expect 76,380 diagnoses and 10,130 deaths in the U.S. alone. Light complexioned persons are twenty times more likely to develop melanoma than those with the darkest complexions, and the risk increases as people age, most likely related to the accumulation of UV radiation exposure.
The two major risk factors for skin cancers are preventable
- exposure to UV radiation; and
- smoking, a lesser risk, known to increase the risk for developing squamous cell skin cancer.
UV radiation increases the risk for all skin cancers — whatever the source
- whether from the sun (especially in the southern states or at high altitudes); or
- from tanning beds (that’s right, tanning beds are not safe, especially for young people)7; or
- from occupational exposures such as in welding.
- NOTE: Even one blistering sunburn, especially in childhood, can double the risk for melanoma.
There are five risk factors for all skin cancers you cannot modify
- fair skin,
- light eyes,
- male gender,
- previous skin cancer, and
- older age.
There are two additional unmodifiable risk factors for melanoma
- more than 50 moles (or unusual moles), and a
- close blood relative with melanoma.
Skin Cancer Survivors’ Testimonials
- I Felt Betrayed, Lied to, and Scared – SkinCancer.org. (n.d.). Retrieved May 2, 2016, from http://www.skincancer.org/true-stories/former-indoor-tanner
“Three weeks later the doctor called to tell me that the ‘freckle’ was a melanoma, the deadliest kind of skin cancer. I dropped the phone, and broke down. I had truly believed what I’d been taught by the industry — that tanning prevented certain cancers and that the industry had the documents and scientists to back up these claims. Instead it seems I’d had a death wish…” - The Scariest Year, the Luckiest Year – SkinCancer.org. (2016, June 12). Retrieved from http://www.skincancer.org/true-stories/the-scariest-year-the-luckiest-year
“Most people are mystified when they hear that I got skin cancer. They didn’t think I was the type. I don’t fit the profile: I am 30 years old with no freckles or moles and have olive skin that never burns…” - How Skin Cancer Changed My Life – SkinCancer.org. (n.d.). Retrieved May 2, 2016, from http://www.skincancer.org/true-stories/how-skin-cancer-changed-my-life
“Now that I’ve had a skin cancer, it’s hard to believe I was so unaware of the danger for so many years. I was happy to be tan and liked the way I looked…”