Basal cell carcinoma (BCC, basal cell skin cancer) is a malignant tumor of the skin, a distinctive feature of which is a pronounced local destruction with almost no risk of metastasis. The low likelihood of metastases causes a relatively favorable prognosis of the disease, provided timely treatment. BCC is usually found at the age of over 35-40 years, equally often in men and women.
Predisposing factors
There is no clear reason for the occurrence of basal cell carcinoma. It is only appropriate to talk about predisposing factors that, to varying degrees, can increase the risk of these neoplasms:
- Excessive insolation: excessive exposure to solar ultraviolet;
- Ionizing radiation;
- The influence of chemical compounds that damage the skin;
- Chronic skin injuries.
Diagnostics
Diagnosis of basal cell cancer is based on a clinical examination, which includes a routine examination of the formation and dermatoscopy. After examination, a biopsy is performed.
Symptoms
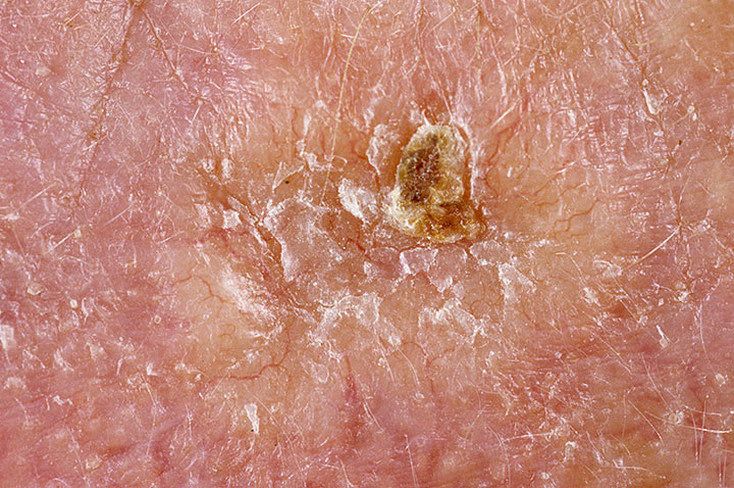
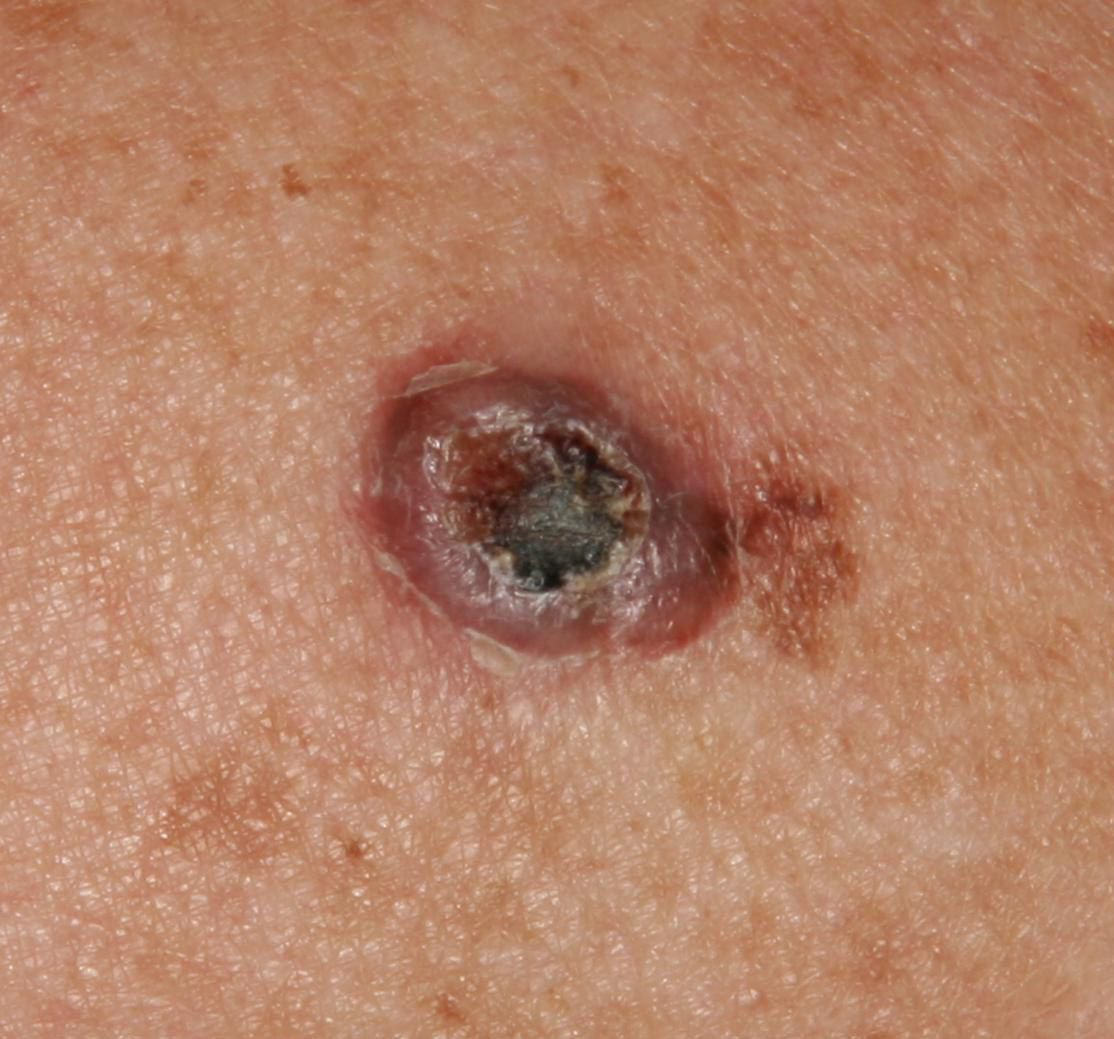
A visual examination of basal cell carcinoma determines a plaque or flattened protrusion protruding above the skin. On the surface, there are tuberosity, wartiness, ulceration, crusts. Upon contact, or even with a minor injury, bleeds easily.
Borders are usually fuzzy (infiltrative growth) and uneven. The shape is often irregular, asymmetric, but sometimes the focus of the BCC is represented by a regular round or oval formation. It may look like a crater-like ulcer with a depression in the center (possibly even below the skin level) or vice versa, protruding above the skin and fixed to it by a wide pedicle formation.
The color is pink, pink-red, with the application of horny masses – gray shades are added. In long-existing forms, foci of tissue necrosis with white-yellow, dirty-gray color may appear on the surface.
Hair growth is absent.
Sizes range from 4 mm to 40 mm. Tumor enlargement is usually slow. In the absence of timely treatment, individual foci can reach large sizes, occupying entire anatomical areas.
On palpation, a more dense formation is defined in comparison with the surrounding skin.
Subjective sensations are usually absent. There is no morbidity with mechanical action on the tumor itself. When subcutaneous structures are involved in the tumor process, pain may appear.
Foci of basal cell carcinoma are located mainly in open areas of the body and areas most often exposed to insolation: head (especially the face), neck, upper limbs, back, lower legs. Slightly less often the area of the chest, abdomen, and thighs.
Dermatoscopic Description
With dermatoscopy, the most reliable symptoms and signs of basal cell carcinoma include:
- Pathological vessels in the form of tree branching;
- Foci of ulceration;
- Spherical inclusions of a pigment of a blue-gray color and a point;
- Unstructured zones of red, pink or white pigmentation;
- Milium-like cysts;
- Chrysalide-like structures in polarized light.
Differential diagnosis
Differential diagnosis is carried out with such neoplasms as:
- Keratoacanthoma;
- Skin horn;
- Seborrheic keratosis;
- Actinic keratosis;
- Bowen’s disease;
- Squamous cell carcinoma;
- Melanoma.
Risks
Despite the fact that basal cell skin cancer is a malignant tumor, the prognosis after timely and correct treatment is relatively favorable. This is due to the almost complete absence of the possibility of tumor metastasis. Only the likelihood of local recurrence remains or the risk of new cases of BCC in a different location increases slightly. Local relapses or multiple tumors, with proper treatment, do not worsen the prognosis.
The risk of relapse in the same place depends on the size of basal cell carcinoma and the depth of its invasion of the skin. As well as the volume and adequacy of surgical treatment.
BCC can appear both on healthy skin and on the background of existing benign or precancerous neoplasms. In the latter case, there is a certain degree of difficulty in timely differential diagnosis and detection of malignant transformation.
In recent years, the incidence of BCC has been increasing: by about 10% in 5 years.
Tactics
If a suspicion is detected or if the first signs of basal cell skin cancer are detected, an oncologist should be consulted. The oncologist conducts additional specifying tests. In the absence of sufficient clinical data for an unambiguous diagnosis, sometimes the tactics of active dynamic observation is chosen. More often, a suspicious lesion or biopsy is performed, followed by histological examination.
With histological confirmation of BCC, a standard list of examinations is assigned to search or exclude the presence of metastases, after which a special treatment plan is formed.
In this regard, in patients with the presence of CCB, the risk of other malignant tumors increases – a regular thorough examination of the skin is recommended. When suspicious neoplasms are detected, a positive role is played by their photo fixation, which will subsequently determine even minor changes in appearance. In the same situations, an examination by a dermatologist or oncologist in the spring and autumn (before the beach season and after it) is indicated. Of great importance is the mapping of skin neoplasms, which greatly simplifies further observation, the search for new formations, or changes to existing ones.
Treatment
The main treatment method is surgical: wide excision of the tumor focus. This is the most effective method with a low risk of local recurrence.
Another effective and universally recognized method is short-focus x-ray therapy (radiation therapy). It is usually used to treat foci up to 20 mm.
The use of other methods of local exposure (laser removal or cryodestruction) even of the earliest forms is unacceptable. The tumor should be removed radically, within healthy skin, without damaging the tumor focus itself. Otherwise, the risk of local relapse increases.
Today, methods are being developed for the local use of cytostatics (chemotherapy). However, there is no unequivocal opinion regarding such treatment due to the fact that these methods increase the duration of treatment of skin cancer, the cost, the damaging effect on the healthy surrounding skin and have dubious radicalism when used improperly. Such treatment should be carried out under the strict supervision of a specialist. On the other hand, local treatment with the help of certified and approved by oncologists means has a good cosmetic result.
Prevention
Prevention of the appearance of basal cell skin cancer and its progression is gentle and careful attitude to the skin:
- Limitation of ultraviolet radiation (tanning bed, solar tanning);
- The use of protective creams during periods of active sun;
- Exclusion of chronic skin trauma;
- Limitation or exclusion of ionizing radiation, occupational hazards;
- Compliance with safety measures when working with skin-damaging factors;
- Personal hygiene and basic awareness of skin tumors.
It also requires regular examination of the skin, timely consultation with a specialist in the event of external changes in skin tumors, and the removal of potentially dangerous neoplasms.

































** Should you identify any copyright infringement regarding the images on this page, kindly reach out to us at info@skinive.com.
Furthermore, please be advised that these photos are not authorized for any purpose.
