Devergie’s lichen is a rare chronic inflammatory skin disease with unknown etiology. The main manifestations of this pathology include peeling and redness of the skin in combination with damage to the hair follicles. Equally common in both men and women, and without emphasis on age.
There are 6 clinical types of Devergie’s lichen:
- Type I is the most common, which is also called the “classic adult type”. This type of Devergie’s lichen has the best prognosis, since up to 80% of cases pass on their own within 3 years;
- Type II – atypical, is a type I variety, which is characterized by atypical onset of the disease in adults;
- Types III, IV, and V are classic, limited, and atypical adolescent Devergie’s lichen;
- Type VI is an HIV-associated type of Devergie’s lichen.
Considering the non-infectious nature of Devergie’s lichen, it is not contagious and is not transmitted from person to person. Devergie’s lichen is usually not inherited, but familial cases associated with a genetic predisposition have been described.
Symptoms of Devergie’s lichen
The main manifestation of Devergie’s lichen is a characteristic pinpoint rash, which in the early stages can be accompanied by the appearance of itching. As the disease worsens, thick skin appears on the palms and soles, followed by peeling, cracks and soreness. This can make walking difficult, and working with your hands causes noticeable discomfort.
Further progression of the rash can cause a fever, severe weakness, and other signs of intoxication. Elements of the rash merge into large red spots.
Signs of the most common Devergie’s lichen (type I):
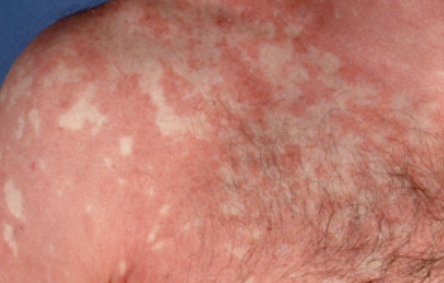
- The rash usually begins suddenly on the scalp and spreads to most of the chest and abdomen;
- The spots are dry, scaly, red with an orange tinge and well-defined edges. Smaller patches may coalesce to cover larger areas of the skin;
- Between the larger red spots, areas of normal skin can often be seen.
The hair follicles on the affected skin areas are enlarged, denser to the touch, with a scaly surface due to hyperkeratosis.
The skin on the palms and soles may thicken and be orange in color. Nails may also thicken with subsequent discoloration and, in severe cases, hair loss.
Type II (atypical adult) accounts for 5% of all cases of Devergie’s lichen and does not have the classic course described above, when the rash begins in the head. Here, the legs are usually immediately affected with thickening of the skin on the palms and soles. Devergie’s lichen type II may be associated with increased hair loss.
Type III accounts for 10% of all cases. The manifestations are similar to those of type I, but they begin in childhood.
Type IV accounts for 25% of cases. Symptoms are similar to those of type II, but are also typical for children.
Type V accounts for 5% of cases. Combines the symptoms of type I and type II, but the disease is noted in several members of the same family. This type has an autosomal dominant inheritance with the manifestation of the first symptoms in childhood. It usually starts with dry skin and blockage of hair follicles, later thickening of the skin on the arms and legs joins.
Type VI occurs in people with HIV and is characterized by red, scaly patches around hair follicles with or without involvement of the palms and soles.
Diagnostics of the Devergie’s lichen
A visual examination is often sufficient to diagnose Devergie’s lichen. However, the diagnosis process can be difficult if the rash is atypical. If the diagnosis is unclear, additional tests may be done to rule out fungal skin lesions (potassium hydroxide (KOH test) or other diseases (culturing, biopsy).
The various types of hairy scalp can look like psoriasis and are often mistaken for psoriasis, especially in the early stages.
Devergie’s lichen treatment
There are no standardized treatment protocols for Devergie’s lichen treatment, as well as specific medications. Topical and systemic therapies are usually used alone or in combination.
For small areas of skin lesions, local treatment is prescribed. Steroid creams and ointments can reduce the severity of symptoms (redness, flaking, itching) but do not change the duration of the illness.
Moisturizing topical medicines are a very important part of the treatment, helping to relieve dryness and restore the skin’s barrier function. Emollients should be used regularly.
In the case of extensive lesions and the occurrence of general symptoms of intoxication, a dermatologist, after assessing the patient’s condition, prescribes systemic treatment. The most commonly used are retinoids, methotrexate, and systemic corticosteroids.
To relieve itching, antihistamines, both local and systemic, can be prescribed. In some cases, phototherapy (light therapy) is used.
If the drugs listed above are ineffective, as well as the progression of the rash, biological drugs can be used that act on specific antibodies that block a certain protein involved in the occurrence of Devergie’s lichen. These drugs include infliximab, ustekinumab, secukinumab, and adalimumab.





















** Should you identify any copyright infringement regarding the images on this page, kindly reach out to us at info@skinive.com.
Furthermore, please be advised that these photos are not authorized for any purpose.
