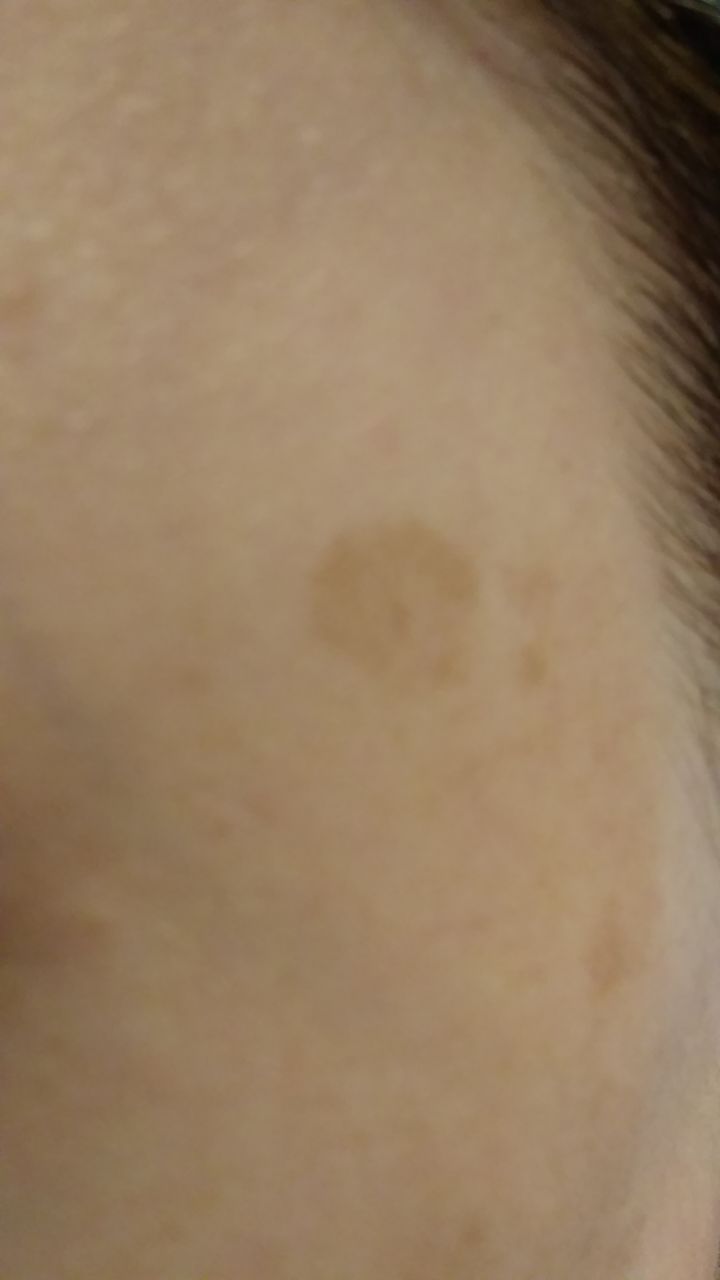
Lentigo (melanin hyperpigmentation, actinic lentigo, sunspots) is a benign skin neoplasm, which is a light brown single multiform spot or a group of many smaller spots, but of the same type. Lentigo usually appears in people over 35 years old, usually under the influence of solar ultraviolet radiation. At a younger age, lentigo is rare (less than 20%), and this is more often associated with metabolic pathology or with hormonal disorders. With age, the risk of lentigo increases: in people over 60, it is found in 90% of people.
Predisposing factors
There is no clear reason for the appearance of lentigo. It is only appropriate to talk about predisposing factors that, to varying degrees, can increase the risk of hyperpigmentation:
- Ultraviolet radiation: artificial or solar ultraviolet leads to excessive production of melanin (skin pigment);
- Hormonal changes: the appearance of lentigo can be affected by hormonal fluctuations in the body (especially sex hormones, thyroid hormones and adrenal hormones);
- Ionizing radiation, viral diseases and injuries can also trigger the appearance or growth of lentigo;
- Genetic factor: the appearance of lentigo may be due to the human genome
- Light skin: I-II phototype of the skin according to Fitzpatrick;
- Age over 35 years.
Diagnostics
Diagnosis of lentigo is based on a clinical examination, which includes a routine examination of the formation and dermatoscopy. If you suspect malignant growth, a biopsy can be performed (excision biopsy, excision of the entire formation).
Symptoms
A visual examination of lentigo determines a spot or group of spots, possibly a slight elevation above the skin (usually not more than 1 mm). A neoplasm can be either symmetrical or irregular in shape (fusion of several spots, a group of separate spots, including multiple spots, occupying entire anatomical areas). The surface is a texture of ordinary skin, small tuberosity (roughness), peeling may be present.
The boundaries of lentigo are clear, but most often uneven (especially large spots, multi-focal). Lentigo coloration varies from light brown to brown. Dark colors are usually absent. The distribution of pigment throughout the formation is uniform. Sometimes there is a gradual decrease in color intensity in the direction from the center to the periphery, or an irregular change of tint over the area of the entire pigment focus. Over time, the color intensity may increase. Sometimes there are shades of gray as a result of keratinization of the upper layers of the epithelium.
Lentigo, as a rule, does not affect hair growth.
The size of the lentigo is very variable: individual spots from 2-3 mm to 3-4 cm, grouped lesions can reach several tens of centimeters.
On palpation of lentigo, there are no features: the consistency of ordinary skin. Subjective sensations are also absent. In long-existing forms, roughness is noted, itching is possible.
Lentigo is located mainly on the face or other open areas of the body. In the elderly, spots can appear on other parts of the body.
Dermatoscopic Description
With dermatoscopy, lentigo is visualized:
- Uniform pigment network – a pattern of hypopigmented holes and uniform lines from light brown to dark brown. The lines are evenly thinning to the periphery of the formation;
- Pseudo-network is a reticulate structure formed by the dermal mouths and hair follicles against the background of diffuse brown pigmentation;
- Ring-granular structures – granular pigmentation surrounding the hair follicles in the form of a regular ring;
- Regular points – are small hyperpigmented round structures that are located in the center or are found on the pigmented lines of the network;
- Diffuse uniform staining of the entire formation.
Differential diagnosis
Differential diagnosis is carried out with such pigmented neoplasms, as:
- Post-inflammatory hyperpigmentation;
- Congenital dermal melanocytosis;
- Halo nevus;
- Spitz Nevus;
- Dysplastic nevus;
- Lentigo melanoma;
- Pigmented basal cell carcinoma;
- Melanoma.
Risks
In the absence of external effects on lentigo (trauma, ultraviolet radiation, ionizing radiation) – the risk of malignant degeneration of lentigo is low and almost comparable to the risk of melanoma on unchanged skin. Signs of a possible malignancy of lentigo: a change in appearance, the appearance of subjective sensations.
Malignant lentigo (Dubreuilh melanosis) is a precancerous condition and on this background, the risk of melanoma is significantly higher.
Tactics
In the absence of any damaging effect on the lentigo, changes in appearance, and subjective sensations, self-control is sufficient at least once a year. If there is mechanical damage to the pigment spot, its active irradiation with ultraviolet or ionizing radiation, as well as if any changes are noticed or previously absent sensations appear, you need to consult a dermatologist or oncologist.
The specialist determines the possibility of further dynamic observation (terms are determined individually) or indications for treatment are set. It is necessary to remove those foci that are subject to constant, chronic trauma to clothing, jewelry, or due to the characteristics of professional employment.
In the case of dynamic observation, photo fixation of the skin neoplasm is of great value, which will subsequently determine even minor changes in the appearance of the pigment neoplasm.
Patients with multiple or large lesions of lentigo are shown an examination by a dermatologist or oncologist in the spring and autumn (before and after the beach season). Such patients are also recommended to compile a map of skin neoplasms, which greatly simplifies further observation, the search for new formations, or a change in existing ones.
Treatment
Since lentigo is most often just a cosmetic defect, approaches, and the need for treatment are discussed individually. If the goal is not to eliminate a cosmetic defect, treatment is not required. Otherwise, small lesions may be removed surgically. Lentigo in the form of multiple of the same type of light spots can be subjected to conservative treatment in the form of various cosmetic procedures.
Any external influences on the lentigo foci (laser treatment, cryodestruction, hardware cosmetology) should be carried out only after examination by a dermatologist or oncologist (ideally after dermatoscopy). In general, the use of destructive methods for pigment lesions is not recommended, since it is not always possible to identify the process of malignant degeneration in a timely manner and with the help of only one clinical examination.
If surgical removal is not possible (due to the lentigo area or patient’s failure), and the elimination of a cosmetic defect becomes a priority – after the treatment, careful visual monitoring of the area where the lentigo focus was previously located is necessary.
Prevention
Prevention of the appearance of lentigo and its malignancy is a gentle and careful attitude to the skin:
- Limitation of ultraviolet radiation (tanning bed, solar tanning);
- The use of protective creams during periods of active sun;
- Exclusion of chronic skin trauma;
- Limitation or exclusion of ionizing radiation, occupational hazards;
- Compliance with safety measures when working with skin-damaging factors;
- Personal hygiene and basic awareness of skin tumors.
It also requires regular inspection of age spots, timely consultation of a specialist in the event of external changes, and the removal of potentially dangerous neoplasms.



















** Should you identify any copyright infringement regarding the images on this page, kindly reach out to us at info@skinive.com.
Furthermore, please be advised that these photos are not authorized for any purpose.
