Actinic keratosis (AK, solar keratosis) is a benign skin tumor in the form of a fuzzy hyperemic spot with keratinization. Actinic keratosis has a high risk of transformation into squamous cell carcinoma of the skin, therefore, refers to an optional precancerous condition. These formations appear, as a rule, over the age of 40 in open areas of the body that are exposed to frequent and prolonged exposure to solar ultraviolet light. Actinic keratosis is characterized by plurality, the area of skin lesion increases with age. Equally common in both men and women.
Predisposing factors
There is no clear reason for the appearance of actinic keratosis. However, solar ultraviolet and increased susceptibility to its damaging effects on the skin of older people are considered the main provocative factor. Due to the fact that the damaging effects of solar ultraviolet radiation have a cumulative effect, AK can appear even many years after active insolation.
Other factors that, to varying degrees, may increase the risk of actinic keratosis include:
- Skin phototypes: Fitzpatrick I-II;
- Albinism;
- Light, red, blond hair color;
- Age over 50;
- The presence of immunodeficiency states: due to the use of immunosuppressants, chemotherapy for cancer, after severe infections;
- Genetic factor: the appearance of AK may be due to the human genome;
- Ionizing radiation, the influence of chemical compounds, chronic injuries can also provoke the appearance or growth of keratosis.
Diagnostics
Diagnosis of actinic keratosis is based on a clinical examination, which includes a routine examination of the formation and dermatoscopy. If you suspect malignant growth, a biopsy can be performed.
Symptoms
A visual examination of actinic keratosis identifies single, multiple, or grouped spots or plaques. The surface of the plaque differs significantly from the texture of ordinary skin: rough, focal covered with crusts, sometimes with signs of erosion and bruising.
The borders are fuzzy and uneven. The shape is irregular, asymmetric. The color is nude, gray, gray-brown with the presence of pink or pink-red shades.
Actinic keratosis, as a rule, does not affect hair growth.
Sizes range from 5 mm to 20 mm. Grouped structures of several plaques can reach 3-4 cm.
On palpation, a hard, dry formation with peeling is determined. Subjective sensations are usually absent or mild itching.
The preferred localization of actinic keratosis is facial skin (especially the protruding parts: the tip of the nose, auricles, frontal tubercles, zygomatic areas). Also, with great frequency, the scalp, neck, upper limbs (the area of the shoulder girdle, and wrist) are affected – those places that are most exposed to insolation.
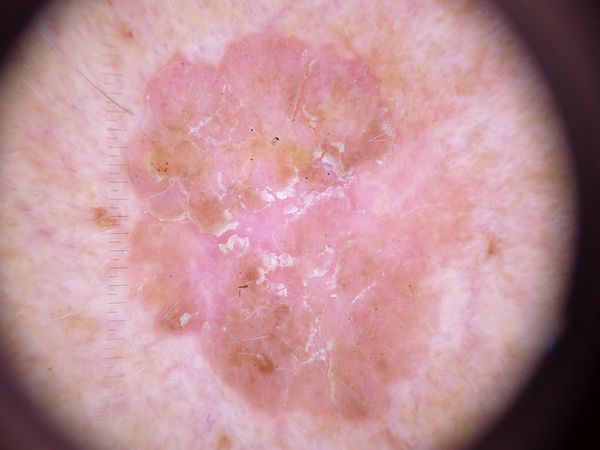
Dermatoscopic Description
With dermatoscopy of actinic keratosis, the following features are visualized:
- Erythema (redness, flushing of the skin);
- Red pseudo-network (reticular structure formed by vessels);
- Superficial keratin flakes and peels;
- White halo around hair follicles;
- Yellowish keratotic plugs (horny masses) in the expanded hair follicles;
- Vascular structures: mainly convoluted and linear;
- Dark brown veins, dots and brown globules in pigmented forms of actinic keratosis.
Differential diagnosis
Differential diagnosis is carried out with such pigmented neoplasms, such as:
- Psoriasis, eczema, dermatitis;
- Seborrheic keratosis;
- Lentigo;
- Post-inflammatory hyperpigmentation;
- Melanosis
- Dysplastic nevus;
- Bowen’s disease;
- Lentigo melanoma;
- Basal cell carcinoma;
- Squamous cell carcinoma;
- Melanoma.
Risks
Actinic keratosis is an optional precancerous condition. The risk of malignant transformation reaches 20%. Malignancy can occur both independently and under the influence of additional external factors (chronic injury, thermal and chemical burns). In the case of malignancy, actinic keratosis is more often transformed into squamous cell (squamous) cancer. Sometimes this happens through a clinically determined phase of Bowen’s disease.
Must be taken into account that patients with severe actinic keratosis have an increased risk of developing a malignant tumor on unchanged skin or near the focus of keratosis. This can complicate the timely detection and differential diagnosis of tumors.
Tactics
In the absence of any damaging effect on the foci of actinic keratosis, changes in appearance and subjective sensations, self-control (or examination with the help of other persons in inaccessible areas) is enough at least once a year. If mechanical damage has occurred, active exposure to ultraviolet or ionizing radiation, as well as if any changes in the keratoma itself are noticed or previous sensations – consultation with a dermatologist or oncologist is needed.
The specialist determines the possibility of further dynamic observation (terms are determined individually) or indications are set for the removal of damaged skin formation. It is necessary to remove those plaques that are subject to constant, chronic trauma to clothing, jewelry, or due to the characteristics of professional employment.
In the case of dynamic observation, photo fixation of skin neoplasms is of great value, which will subsequently determine even minor changes in appearance.
Patients with actinic keratosis require an examination by a dermatologist or oncologist in the spring and autumn (before and after the beach season). Such patients are recommended to compile a map of skin neoplasms, which greatly simplifies further observation, the search for new formations, or a change in existing ones.
Treatment
Due to the fact that actinic keratosis has a rather high risk of transformation into squamous cell carcinoma, along with active dynamic observation, AK treatment is also indicated. Any effects on the foci of keratosis should be carried out only after the exclusion of the fact of malignancy (after examination by an oncologist, dermatoscopy, or biopsy).
First of all, it is necessary to protect the skin from UV radiation: clothing, hats, limiting insolation, sunscreens. These measures significantly reduce the progression of keratosis and its malignant degeneration.
Possible local removal of plaques using local destruction methods (laser, cryodestruction, diathermocoagulation). The use of such methods is also not recommended if it is impossible to conduct a clear differential diagnosis with neoplasms of a pigmented nature (pigmented, dysplastic and other nevi).
Surgical treatment by excision is rarely used due to the frequent presence of a large number and large sizes of foci of keratosis, as well as cosmetic consequences in the form of scars. However, this method has an advantage in cases where it is difficult to exclude malignancy.
There are a number of drugs and techniques that can also be used for topical use in the treatment of actinic keratosis:
- 5-fluorouracil + salicylic acid;
- Hyaluronic acid + diclofenac sodium;
- Imiquimod;
- Ingenol Mebutat;
- Photodynamic therapy;
- Combined procedures in combination with cosmetic products.
However, the application of these methods should be carried out only under the careful and long-term supervision of specialists, it does not always have unambiguously proven efficacy, side effects, high risks of relapse and low availability for a wide range of patients.
Prevention
Prevention of the appearance of actinic keratosis and its malignancy is gentle and careful attitude to the skin:
- Limitation of ultraviolet radiation (tanning bed, solar tanning);
- The use of protective creams during periods of active sun;
- Exclusion of chronic skin trauma;
- Limitation or exclusion of ionizing radiation, occupational hazards;
- Compliance with safety measures when working with skin-damaging factors;
- Personal hygiene and basic awareness of skin tumors.
It also requires regular examination of keratosis foci, timely consultation of a specialist in the event of external changes, and the removal of potentially dangerous neoplasms.



















** Should you identify any copyright infringement regarding the images on this page, kindly reach out to us at info@skinive.com.
Furthermore, please be advised that these photos are not authorized for any purpose.
