Lentigo melanoma is an aggressive malignant tumor. It develops from melanocytes (cells containing the pigment melanin) on the background of Dubreus melanosis. Lentigo melanoma is typical for the elderly age and often appears in open areas of the body (face). There is a long course and a relatively favorable prognosis (when compared with other forms of melanoma) with timely treatment. In the structure of all melanomas, the incidence of lentigo-melanoma is about 5%.
The aggressiveness of lentigo-melanoma is due to the ability of this tumor to frequent relapses and metastasis in almost all organs. The metastasis pathway can be either lymphogenous or hematogenous. The rapid progression of melanoma also depends on the state of the body’s natural antitumor immunity.
Predisposing factors
Most often, lentigo melanoma appears over the age of 50 years. At an earlier age is rare.
Various factors lead to the transformation of normal melanocytic cells into malignant melanoma cells.
Lentigo melanoma usually appears against the background of Dubreus melanosis, a precancerous skin disease that is a pigmented, light brown, multiform spot. Dubreus melanosis develops under the influence of active exposure to solar ultraviolet, adverse weather conditions for the skin, and chronic injury.
There are a number of other factors that, to varying degrees, can increase the risk of lentigo-melanoma (malignancy of Dubreus melanosis):
- Natural (sun) and artificial ultraviolet;
- White/fair skin (I-II phototypes of the skin), the presence of pink freckles;
- Blue, gray or green eyes;
- Blond, red hair;
- Frequent sunburn, including a medical history (especially dangerous sunburn up to 14 years old);
- A burdened hereditary history of melanoma (genetic factor);
- Previously transferred melanoma;
- Age over 50;
- Sporadic or chronic injury to foci of melanosis.
Diagnostics
Diagnosis of lentigo melanoma is based on a clinical examination, which includes a routine examination of the formation and dermatoscopy. The final decision in the diagnosis is only the result of histological examination. In addition to examining the tumor itself, diagnostics of regional and distant metastasis zones is carried out.
Symptoms
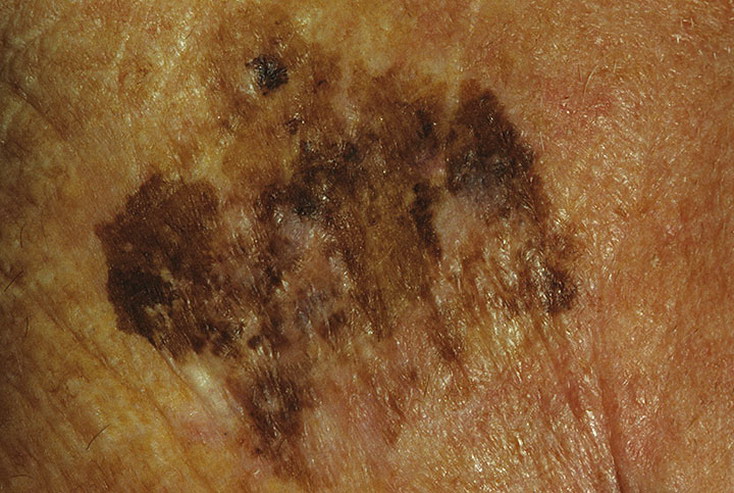
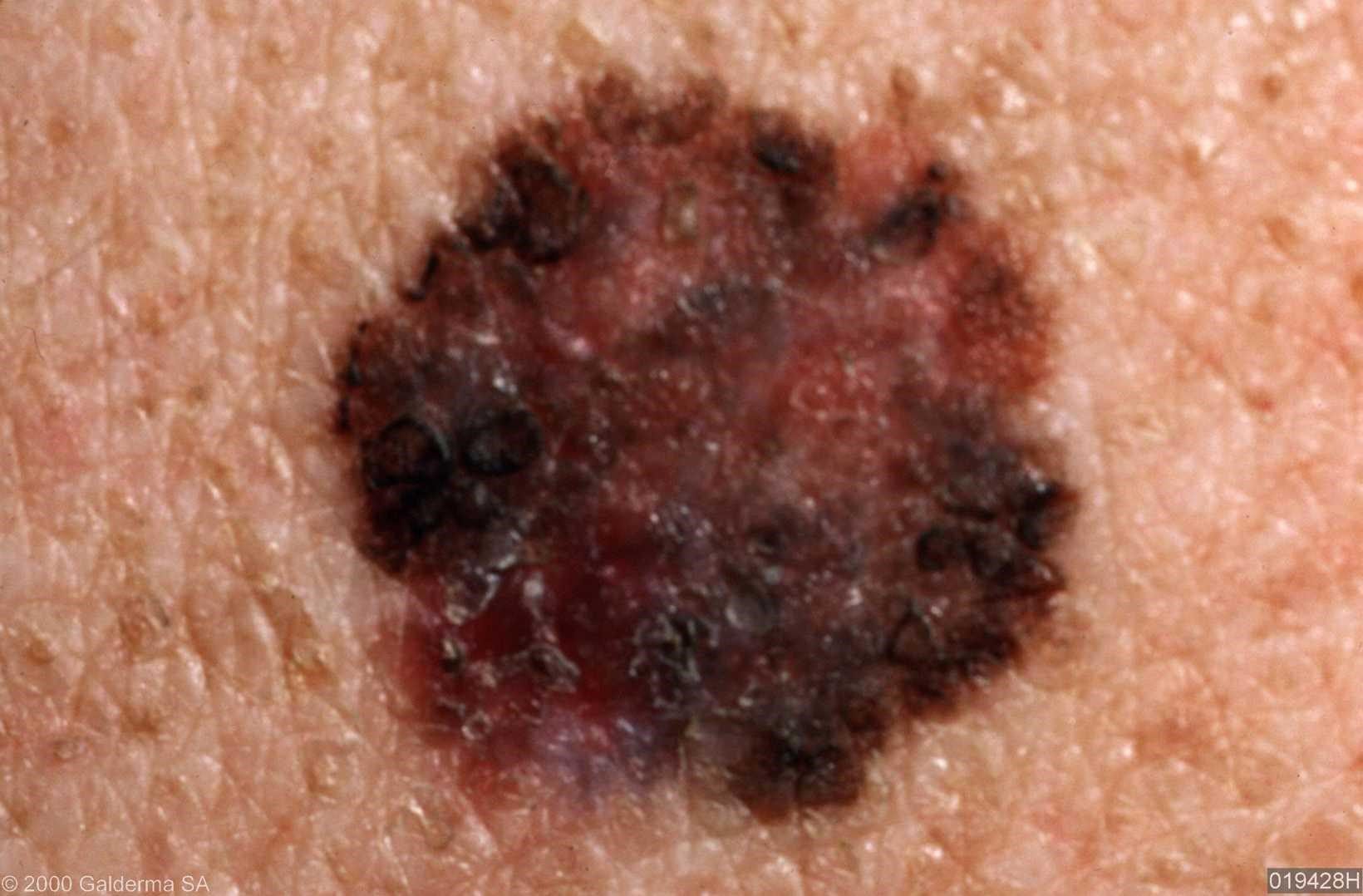
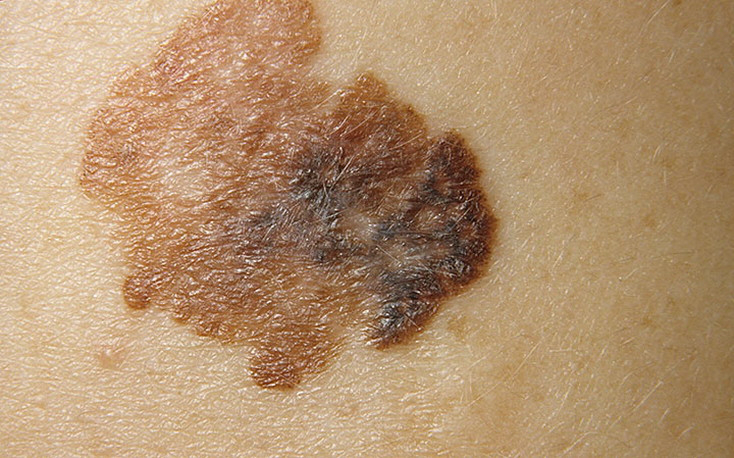
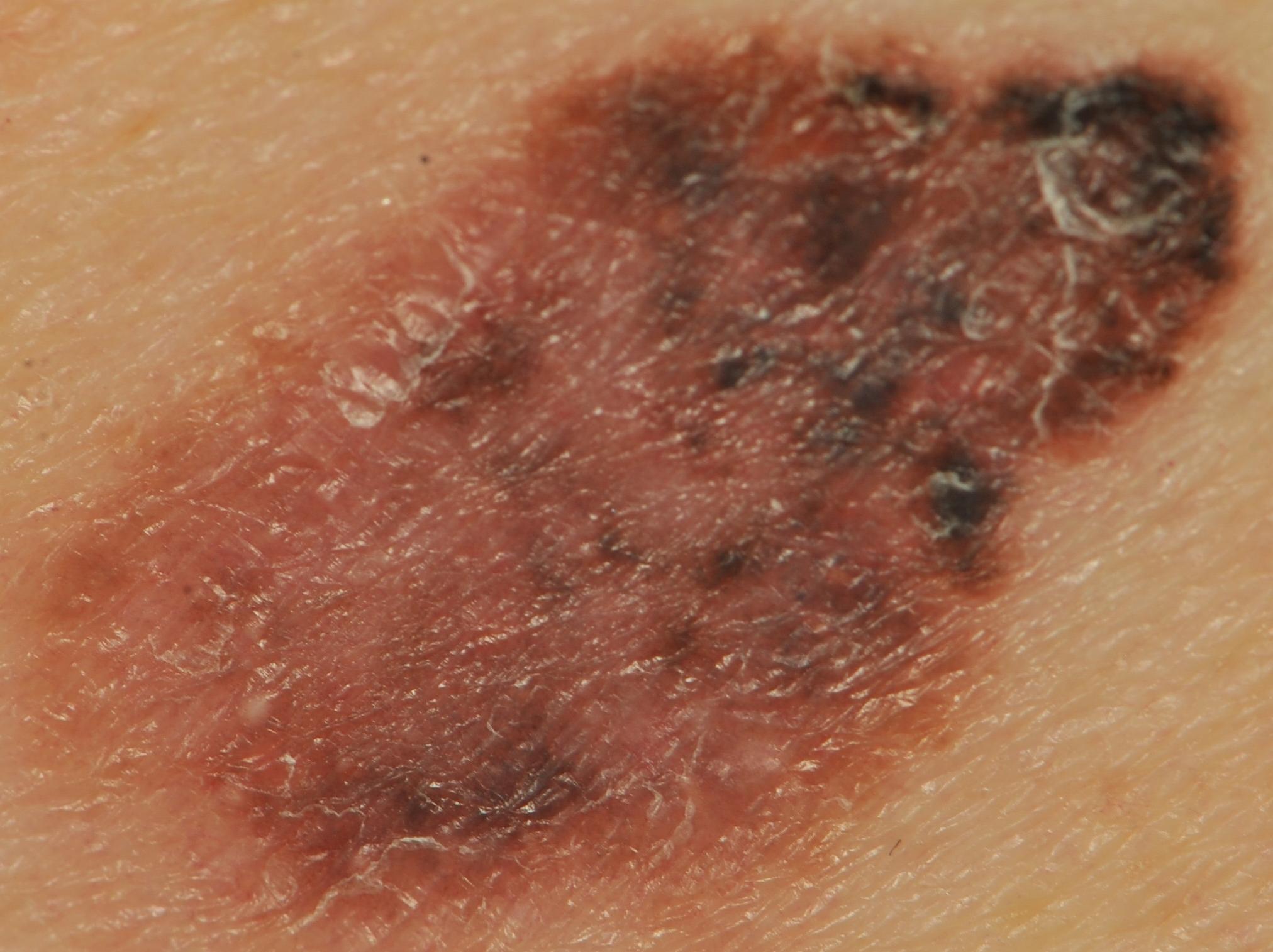
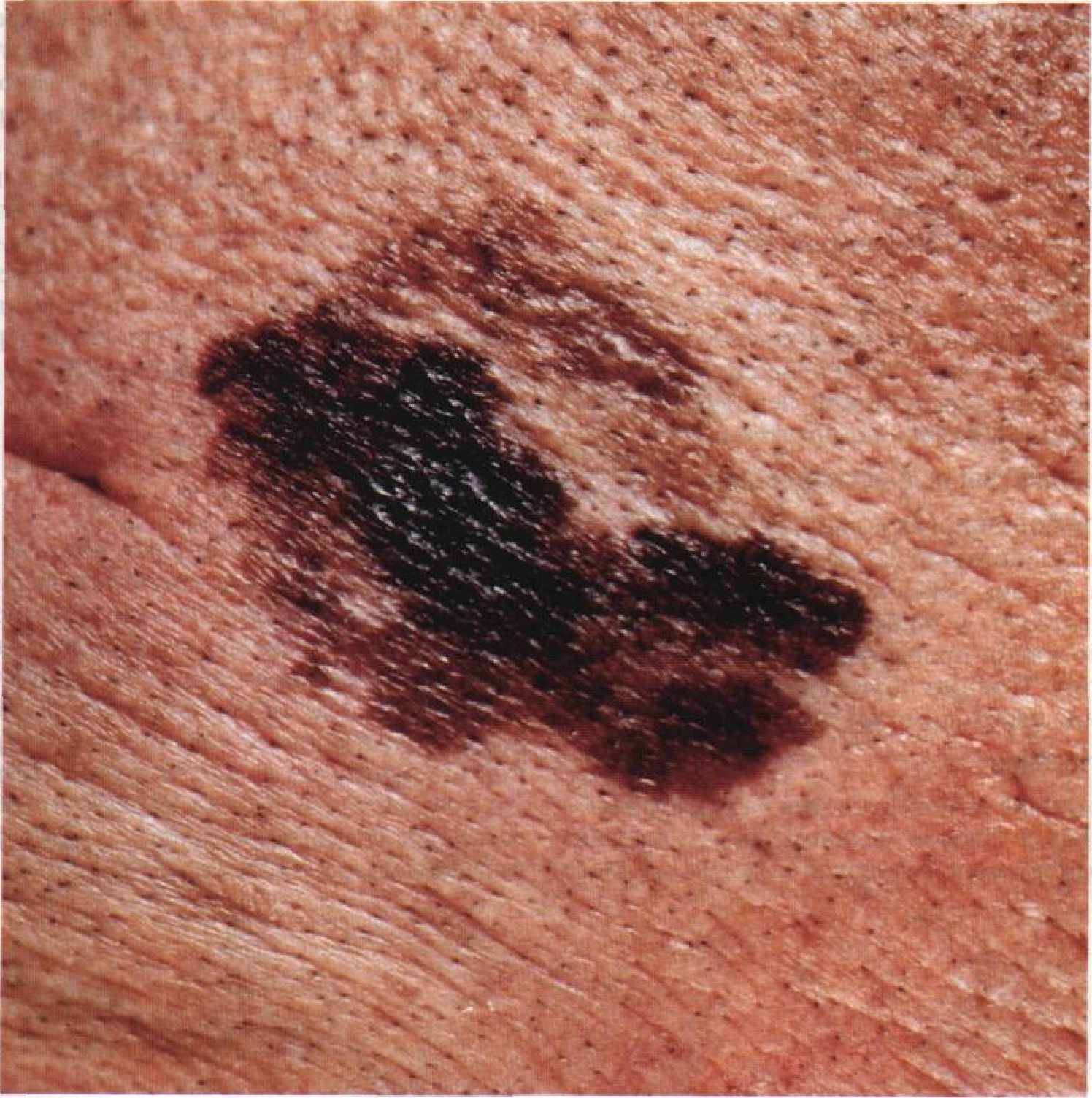
On visual inspection of lentigo-melanoma, a multiform formation in the form of a spot is determined. The surface of melanoma is usually different from the texture of ordinary skin. Only in the very early stages (zero or first) the skin pattern can not be disturbed. In other cases, a rougher surface, peeling, small tuberosity is noted. In advanced cases, an exophytic component appears, weeping, ulceration, bleeding.
Visual assessment of pigmented lesions suspicious of lentigo melanoma is primarily carried out using the ABCDE system (Friedman, 1985):
A – asymmetry, asymmetry of the tumor;
B – border, the state of the edge of the tumor;
C – color, tumor pigmentation;
D – diameter, tumor size;
E – evolving, the evolution (change) of a tumor over time.
Asymmetry is an irregular form of a pigmented neoplasm. It is determined by drawing a conditional line through the center of the tumor, while one half will not be a mirror image of the other half.
The edges of lentigo-melanoma (border with healthy skin) are uneven. In surface forms, the edge is usually clear (favorable factor), when an invasion appears (vertical growth, “immersion” in the skin), the edge becomes less clear, blurred (unfavorable factor).
The color of lentigo melanoma is quite variable within the formation. The simultaneous presence of various shades of brown is possible: from light brown to dark, up to black. Usually, especially in early forms, shades of brown (coffee) color prevail. Over time, the proportion of dark areas increases. The distribution of the pigment is heterogeneous (color heterogeneity over the entire area), asymmetric, with areas up to the complete absence of pigment (areas of regression, unfavorable factor). In addition to brown, other colors or their shades (polychrome) may be present: blue, blue, pink-red, white.
The sizes of detected foci of lentigo-melanoma are usually more than 10 mm due to the fact that this type of malignant tumor appears against the background of an existing pigment formation. Smaller foci, due to long horizontal growth and small thickness of the tumor, are clinically difficult to determine.
The behavior of lentigo melanoma over time is rather mixed. Most often, this is a slow increase in the area of the tumor due to the long, stretching for years, phase of horizontal growth. Acceleration is observed during the transition to the phase of vertical growth (deep into the skin). The evolution (change) of pigment formation also includes:
- The loss of previously present hair in the area of the age spots;
- The appearance of subjective sensations (itching, burning, tingling);
- Increase in tumor density;
- Surface changes (smoothing of the skin pattern, the appearance of tuberosity, roughness, ulceration, cracks or exophytic component);
- Redness around the pigmented neoplasm;
- The rapid disappearance of part or all of the pigmentation, especially after ultraviolet radiation.
For later and neglected lentigo melanomas, it is typical:
- The appearance of nearby similar, but smaller foci (intradermal metastases);
- The presence of enlarged and dense lymph nodes along the lymphatic vessels (regional metastasis zone).
The presence of at least one of the above symptoms is already an indication for consultation with a dermatologist or oncologist. The presence of three signs at the same time – the probability of lentigo-melanoma reaches 80% or more.
The main localization of lentigo-melanoma is the face or other exposed areas of the body. The appearance of lentigo-melanoma in other anatomical areas is very rare.
Dermatoscopic Description
With dermatoscopy of lentigo-melanoma, multicomponentity is visualized (the simultaneous presence of a large number of different pathological patterns):
- Pigment network heterogeneity (atypical pigment network) – different intensity and eccentricity;
- Irregular stripes (mainly club-shaped);
- The presence of irregular inclusions of points and globules against the background of the pigment network (eccentric clusters);
- Globules of various shapes, sizes and colors;
- Asymmetry in color, structure and shape;
- Uneven edges;
- Peripheral radial radiance;
- Polychrome (3 colors);
- The presence of hypopigmentation zones and structureless zones, regression structures (unfavorable factor);
- Blue and white veil;
- Pathological vascular pattern (adverse factor).
Differential diagnosis
Differential diagnosis is carried out with such neoplasms as:
- Congenital dermal melanocytosis;
- Pigmentary nevus;
- Hemangioma (especially with vascular thrombosis);
- Blue nevus;
- Spitz Nevus;
- Dysplastic nevus;
- Lentigo;
- Pigmented basal cell carcinoma.
Risks
Lentigo melanoma is one of the most dangerous malignant tumors. In the world, approximately every 7 years, there is a double increase in the number of primary cases of melanoma. This is due, first of all, to an increase in the intensity of insolation and to a more frequent appearance of people in climatic zones unusual for their skin.
The appearance of lentigo-melanoma against the background of an already existing pigment neoplasm (Dubreus melanosis) to some extent complicates the timely differential diagnosis and detection of malignant transformation.
Despite the fact that melanoma is approximately 10 times less common than other malignant skin tumors, mortality in the first case is 3.5 times higher.
Tactics
If a suspicion is detected or the first signs of lentigo-melanoma are detected, an oncologist should be consulted. The oncologist conducts additional specifying tests. In the absence of sufficient clinical data for an unambiguous diagnosis, sometimes the tactics of active dynamic observation is chosen. Most often, excision of a suspicious lesion is performed, followed by histological examination.
When confirming lentigo-melanoma (clinically or histologically), a standard list of examinations is assigned to search for or exclude the presence of metastases, after which a special treatment plan is formed.
Treatment
In most cases, the treatment is surgical. Standard practice is a wide excision of melanoma under anesthesia or conduction anesthesia (if tumor localization allows this). If metastases are detected in regional lymph nodes, lymph dissection is performed (removal of the entire block of regional lymph nodes). If distant metastases are detected, the treatment regimen is selected individually. For this, the oncologists’ arsenal has quite effective chemotherapy, immunotherapy, radiation therapy regimens, as well as the possibility of surgical removal or minimally invasive therapy of metastases.
Treatment of lentigo-melanoma (even the earliest forms) with local destruction methods (laser removal or cryodestruction) or removal under local anesthesia is unacceptable.
Prevention
Prevention of the appearance of lentigo-melanoma is a gentle and careful attitude to the skin:
- Limitation of ultraviolet radiation (natural (sun) and artificial);
- The use of protective creams during periods of active sun;
- Exclusion of chronic skin trauma;
- Limitation or exclusion of ionizing radiation, occupational hazards;
- Compliance with safety measures when working with skin-damaging factors;
- Personal hygiene and basic awareness of skin tumors.
It also requires regular examination of all pigmented neoplasms, timely consultation of a specialist in the event of external changes, and the removal of potentially dangerous tumors.




















** Should you identify any copyright infringement regarding the images on this page, kindly reach out to us at info@skinive.com.
Furthermore, please be advised that these photos are not authorized for any purpose.
